42 yrs old patient with abdominal pain
January 18,2023
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.

A 42 year old male patient, farmer by occupation, resident of Nalgonda, came to our hospital with the cheif complaints of-
Fever since 3 days, Abdominal pain since 3 days, Shortness of breath since 2 days and Cough with sputum since 2 days.
Date of admission:-10/01/2023
History of present illness:-
Patient was apparently assymptomatic 3 days ago and then he noticed fever which was sudden in onset, gradually progressive, high grade, associated with chills, rise of temperature during nights and subside by early morning
Pain in the hypochondrium and epigastric region since 3 days which was sudden in onset, gradually progressive, non-radiating and dull-aching type of pain. No aggravating and relieving factors.
Pain was not relieved by medication.
Shortness of breath (Grade 2) since 2 days and cough with expectorant since 2 days mucoid in consistency and also associated with chest pain.
Loss of appetite since 3 days
No history of loose stools, vomitings, weight loss.
History of past illness:-
No history of similar complaints in the past.
Not a known case of diabetes, hypertension, tb, epilepsy, asthma.
Personal history:-
Diet :- mixed diet.
Appetite:-Decreased
Sleep:-Adequate
Bladder and bowel movements:- Regular
Chronic alcoholic(90ml) since 5 yrs and chronic smoking since 20 years(1 packet).
Drug history:-
No known relevant drug allergies
Family history:-
No significant family history.
General examination:-
Patient is conscious, coherent, cooperative and well oriented to time, place and person.
No Pallor
No Icterus
No Clubbing
No Cyanosis
No Lymphadenopathy
No Edema of feet
No Malnutrition
Vitals:-
Temperature-98.6 F
Pulse rate-104 bpm
RR-32 cpm
BP-110/70 mm/hg
SPO2-97% at room temperature
SYSTEMIC EXAMINATION:-
RESPIRATORY SYSTEM-
Upper Respiratory Tract:
No Halitosis
No oral thrush
No postnasal drip
No Pharyngeal deposits
Mild dental caries
No deviated nasal septum
Lower Respiratory Tract:
Inspection-
Chest is asymmetrical
Trachea-Midline
No drooping of shoulders
No supra clavicular/infra clavicular hollowing
No sinuses
No scars
No dilated veins
Asymmetric chest expansion
MOVEMENT OF CHEST:
RIGHT LEFT
SUPRACLAVICULAR :. SYM. SYM
MAMMARY:. ASYM ASYM
INFRAMAMMARY :. ASYM. ASYM
AXILLARY:. SYM. SYM
INFRA AXILLARY :. SYM. SYM
SUPRASCAPULAR :. SYM. SYM
SCAPULAR :. SYM. SYM
INFRASCAPULAR:. SYM. SYM
Abdomino- thoracic movement with respiration
Palpation-
Chest- Asymmetrical chest movements
measurements-
Inspiration-30 cms
Expiration-29.5 cms
Difference-0.5 cms
Hemithorax-15 cms
Trachea-Midline
Supraclavicular - normal
Infraclavicular - normal
Mammary - normal
Inframammary - normal
Axillary - normal
Infraaxillary - normal
Suprascapular - normal
Interscapular - normal
Infrascapular - vocal and tactile fremitus heard
Percussion-
Non-tender
Supraclavicular - normal
Infraclavicular - normal
Mammary - dull sound heard
Inframammary - dull sound heard
Axillary - normal
Infraaxillary - normal
Suprascapular - normal
Interscapular - normal
Infrascapular - normal
Ascultation-
Breath sounds -absent
Added sound - rub
ABDOMEN-
Oral cavity examination-
Hyperpigmentation of gingiva is seen
Plaque and claculus are present
No gingival enlargement
No Halitosis
No oral thrush
No postnasal drip
No Pharyngeal deposits
Mild dental caries
Abdomen examination-
Inspection-
Shape of the abdomen-Scaphoid
Flanks - full
No abdominal distention visible
Umbilicus-Position-Midline
Shape-Inverted
No scars
No sinuses
No scratch marks
No puncture marks
No dilated veins
No visible peristalsis
Palpation-
Liver-Non tender
No palpable lumps
Soft
Positive bowel sounds
Spleen-Non palpable
Percussion-
No fluid thrill
No shifting dullness
Ascultation-
Bowel sounds heard - 3/ min
No bruits heard
CENTRAL NERVOUS SYSTEM-
Sensory system examination
Pain-Pain on Percussion
Temperature-Able to feel the temperature
Fine Touch-Able to differentiate
Crude Touch-able to differentiate
Pressure-Able to differentiate
Provisional diagnosis:-
Liver abscess with Pleural Effusion
Investigations-
Hemogram
CUE
Blood urea
Serum electrolytes
Serum creatinine
Urine protein/creatinine ratio
Random blood sugar
Fasting Blood Sugar
Post lunch blood sugar
HbA1C(Glycated hemoglobin)
Blood parasites
LFT
Chest X-Ray
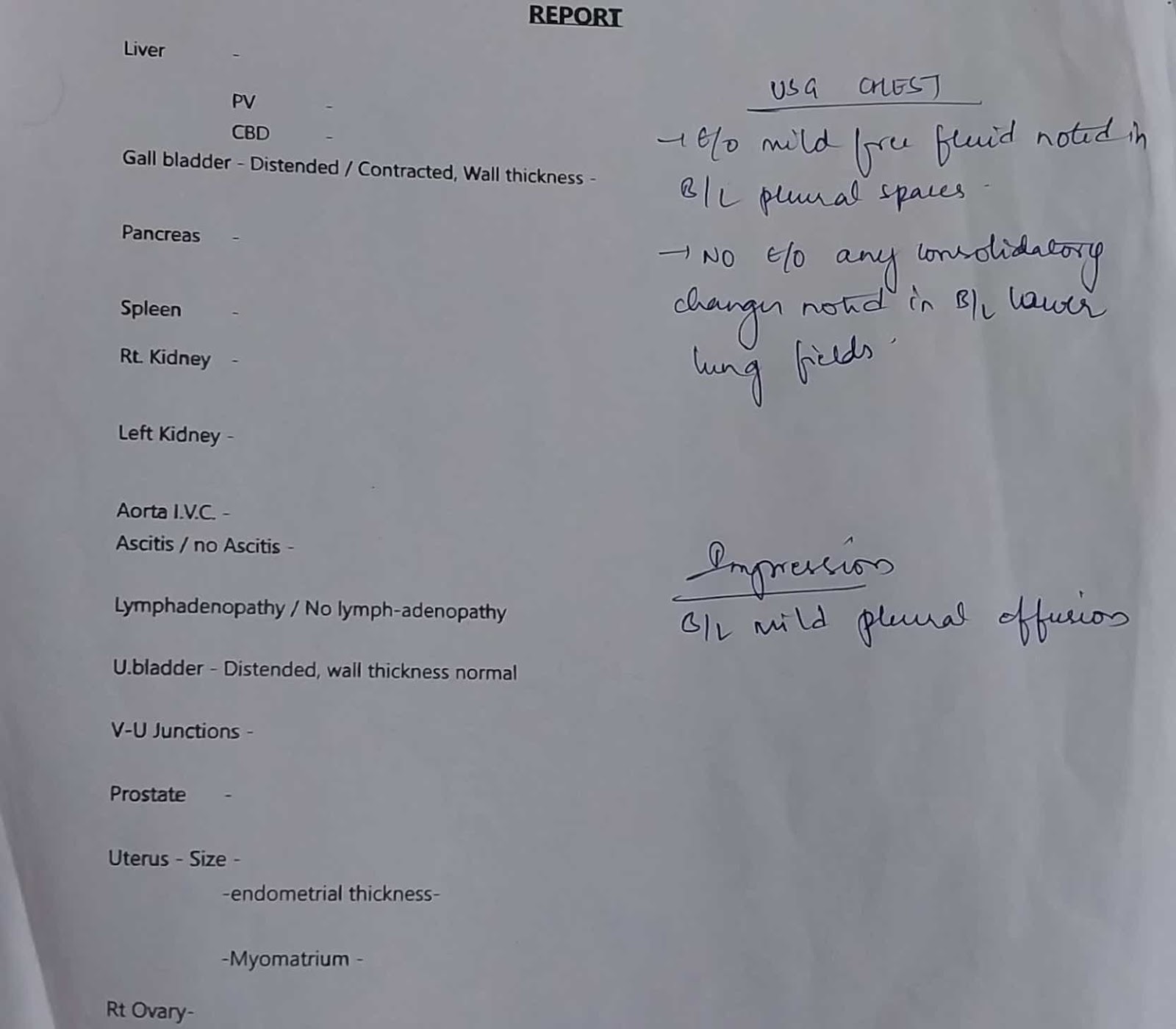
USG Chest
USG Abdomen
ECG
Colour Doppler 2D Echo
13/01/23
Serum creatinine
11/01/23
12/01/23

Urine protein/Creatitine ratio
12/01/23
Random Blood Sugar
10/01/23
Fasting Blood Sugar
11/01/23
Post Lunch Blood Sugar
12/01/23
HbA1C
11/01/23
Blood Parasites
10/01/23

Final diagnosis:-
Liver abscess with Pleural Effusion
Treatment:-
IV Fluids NS RL @ 100 ml/hr
Inj. Monocef 2gm/IV/BD
Inj. Metrogyl 750mg/IV/TID
Inj. Pantop 40mg/IV/TID
Inj. Optineuron lamp 100ml NS/IV/OD
Inj. Thiamine 200mg in 100ml NS/IV/BD
Tab. Dolo 650mg PO/6th hourly
Inj. Neomol 1gm/IV/SOS





























Comments
Post a Comment